Eczema: A Complete Guide to Understanding and Managing Your Skin
Dr. Roisins advice on Eczema and what you need to know

Introduction
Did you know that eczema affects 1 in 5 children and 1 in 10 adults in the UK? This common skin condition, also known as atopic dermatitis, can significantly impact quality of life. Often beginning in childhood, eczema can also appear for the first time in adults. Eczema causes dry, itchy, and inflamed skin, and managing it can sometimes feel overwhelming—especially when flare-ups seem to appear out of nowhere. However, with the right knowledge and tools, you can take control of your skin. In this post, we’ll explore everything you need to know about eczema in adults, from identifying triggers to finding the best treatments for relief.
Understanding Eczema: What You Need to Know
Eczema is a chronic, inflammatory skin condition that affects people of all ages. The most common type is atopic eczema, which is linked to an overactive immune response. The term “atopic” refers to a group of conditions—eczema, asthma, hay fever, and food allergies—that often occur together.
In people with eczema, the skin’s protective barrier doesn’t function as it should. This barrier normally keeps moisture in and irritants out, but when it’s disrupted, the skin becomes dry, sensitive, and prone to inflammation. This leads to the hallmark symptoms of eczema: redness, itching, and sometimes cracking or oozing.
For most people, eczema involves periods of calm followed by flare-ups, where symptoms worsen.
Uncovering the Root Causes of Eczema
Eczema is a complex condition with no single cause. It involves a mix of genetic, environmental, and immune system factors:
- Genetics: About 70% of people with eczema have a family history of atopic conditions like asthma or hay fever (NHS, 2024).
- Immune System: In eczema, immune cells release inflammatory chemicals (cytokines), causing itching and irritation.
- Environmental Factors: Urban living, pollution, tobacco smoke, and reduced exposure to microbes in early life can increase eczema risk.
Is Eczema Caused by an Allergy?
This is a common and important question we encounter in clinical practice. While eczema itself isn’t directly caused by an allergy, research shows that having eczema can increase the likelihood of developing allergies later in life.
This phenomenon is known as the Atopic March. It describes a common progression seen in some children: it starts with eczema in infancy, followed by the development of other allergic conditions like asthma, hay fever, or food allergies as they get older.
Rather than allergies causing eczema, it seems that eczema may act as a kind of “gateway,” making the immune system more sensitive to allergens over time. This doesn’t mean everyone with eczema will develop allergies, but it highlights the importance of early skin care and monitoring for other atopic conditions.
Why Does Eczema Flare Up?
Eczema flare-ups occur when the skin’s natural barrier weakens, leading to irritation and inflammation. While triggers vary from person to person, the key to managing flares lies in understanding your unique triggers—whether it’s stress, weather changes, or irritants.
Common Triggers Include:
- Dry Skin: When the skin loses moisture, it becomes more prone to irritation and inflammation.
- Irritants: Everyday products like soaps, detergents, and fragrances can strip the skin of its natural oils.
- Allergens: Pollen, pet dander, dust mites, and certain foods can trigger an immune response.
- Weather Changes: Cold, dry air in winter or hot, humid conditions in summer can aggravate symptoms.
- Stress: Emotional stress can weaken the skin’s barrier and increase inflammation.
- Infections: Bacterial or viral infections, such as staphylococcus, can worsen eczema.
Quick Tips to Identify Your Triggers:
- Keep a symptom diary to track flare-ups and potential triggers.
- Notice patterns related to weather, diet, or stress.
- Consult your GP or dermatologist for further advice, or allergy testing if needed.
The Itch-Scratch Cycle and Its Impact
Itching is one of the most challenging aspects of eczema. Scratching may provide temporary relief but damages the skin barrier, worsening inflammation and itching—a sequence known as the Itch-Scratch Cycle.
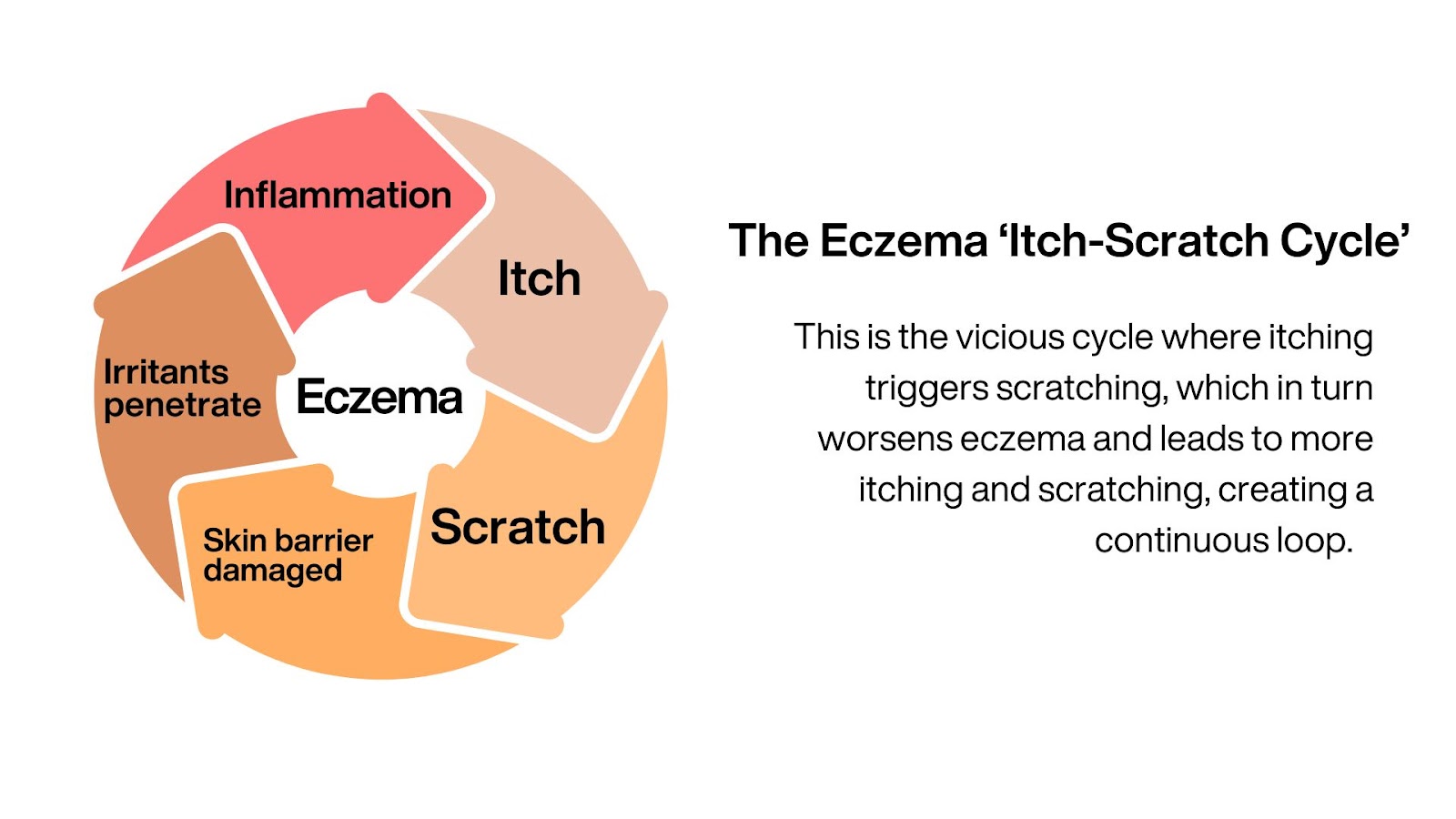
Itching isn’t just a physical symptom—it can also impact mental health. People with eczema can feel self-conscious about visible flare-ups, leading to embarrassment, low self-esteem, or social withdrawal. The constant discomfort and appearance of eczema can contribute to stress, anxiety, and sleep issues, creating a cycle that worsens symptoms.
How to Manage Eczema: Practical Tips for Healthier Skin
Managing eczema is all about balancing daily care with targeted treatments during flare-ups. With the right approach, you can take control of your skin and reduce the impact of eczema on your life. Here’s how to get started:
1. Maintenance Treatment: The ‘ABC’ Approach
Think of maintenance treatment as your daily skincare foundation. Most doctors recommend the ‘ABC’ approach to keep eczema under control:
- A: Avoid Triggers
Identify and avoid irritants like harsh soaps, synthetic fabrics, or allergens. Keeping a symptom diary can help pinpoint what causes your flare-ups.
- B: Bland Moisturisers
Use emollients (medical moisturisers) 3-4 times daily to keep your skin hydrated and protected.
- C: Control Inflammation
Use prescribed treatments like topical steroids during flare-ups to calm inflammation and prevent worsening symptoms.
2. Flare-Up Treatment: Taking Control When Symptoms Worsen
During a flare, the skin becomes more red, itchy, and inflamed. Here’s how to manage it effectively:
- Moisturise More Frequently: Increase your use of emollients to soothe and protect the skin.
- Use Topical Steroids: Apply these to reduce inflammation, itching, and redness. For best results, apply them 20-30 minutes after your emollient to allow the emollient to absorb first.
- Avoid Scratching: Keep your skin cool, wear soft, breathable fabrics, and consider antihistamines to reduce itching. Breaking the itch-scratch cycle is key to preventing further damage.
Why Emollients Are Essential for Eczema
Emollients are the cornerstone of eczema care. Unlike normal moisturisers, which simply add moisture to the skin, emollients do much more:
- Repair the Skin Barrier: Emollients fill in the gaps between dry, cracked skin cells, helping to restore the skin’s natural protective barrier.
- Lock in Moisture: They form a protective layer on the skin’s surface, preventing water loss and keeping the skin hydrated for longer.
- Soothe and Protect: By reducing dryness and irritation, emollients help prevent the itch-scratch cycle that can worsen eczema.
For best results, use emollients liberally and frequently—the average adult with eczema should aim for about 500g per week. Apply them all over the skin, not just on affected areas, to keep your skin barrier strong and resilient.
When to See a Doctor
While mild eczema can often be managed at home, it’s important to seek medical advice if:
- Your symptoms are severe or not improving with treatment.
- You suspect a skin infection (e.g., crusting, fluid-filled spots, or feeling unwell).
- Eczema is affecting your sleep, mental health, or daily life.
If you suspect a skin infection, contact your GP or pharmacist immediately.
Online GP Appointments for Eczema Management
At Online Doctor, we understand the challenges of dealing with eczema and offer convenient online appointments to support you. Our healthcare professionals provide personalised advice, recommend eczema management strategies, and, if necessary, prescribe further treatment options.
Booking an online appointment is quick and easy. Simply select a time that suits you, and connect with a qualified professional from the comfort of your home.
Final thoughts
Eczema can be a challenging condition, but with the right knowledge and tools, you can take control of your skin health. By understanding your triggers, following a consistent skincare routine, and seeking professional advice when needed, you can reduce flare-ups and improve your quality of life.
If you’re struggling to manage your eczema, book an online GP appointment today for personalised advice and support.
References
- NHS. (2024). Atopic Eczema. Available at: https://www.nhs.uk/conditions/atopic-eczema/
- National Eczema Society. (2023). Emollients Factsheet. Available at: https://eczema.org/wp-content/uploads/Emollients-Jun-23.pdf
Dr Roisin O’Regan